Cancer staging imaging employs CT, MRI, and PET scans to visualize tumors, aiding oncologists in treatment planning. These technologies offer unique benefits but carry radiation risks, requiring careful dosing and protocol adherence. Future research focuses on safer alternatives, AI-assisted analysis, and personalized medicine to minimize exposure while enhancing diagnostic accuracy.
Cancer diagnostic scans play a pivotal role in understanding and treating the disease. However, concerns around radiation exposure during these procedures are valid. This article delves into the world of cancer staging imaging, exploring various techniques used, the associated risks and benefits of radiation exposure, and strategies to minimize those risks. We also discuss future directions aimed at enhancing safety measures, ensuring accurate cancer diagnosis without compromising patient well-being.
Understanding Cancer Staging Imaging Techniques
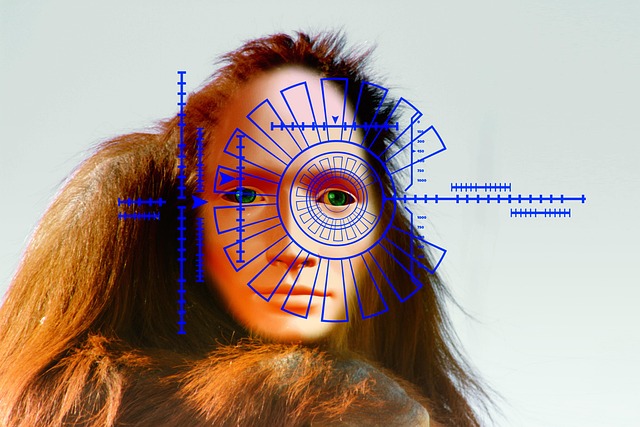
Cancer staging imaging plays a crucial role in understanding the extent and spread of cancer within the body. These advanced techniques, such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET), provide detailed visualizations of internal structures. By analyzing these images, medical professionals can accurately determine the stage of cancer, identifying whether it has invaded nearby tissues or metastasized to distant organs.
This process is vital in devising an effective treatment plan as it helps oncologists assess the severity and location of tumors. Each imaging modality offers unique advantages; for instance, CT scans excel at providing high-resolution cross-sectional images, while MRI delivers detailed anatomical information without ionizing radiation. PET scans, on the other hand, help detect metabolic changes associated with cancerous cells. Understanding these staging imaging techniques is essential for healthcare providers to make informed decisions and provide personalized care to patients with cancer.
The Benefits and Risks of Radiation Exposure
While radiation exposure is an essential tool in cancer diagnostic scans, especially for cancer staging imaging, it’s crucial to balance its benefits against potential risks. Radiation plays a pivotal role in detecting and diagnosing various types of cancers at early stages when treatment outcomes are often better. It helps identify tumors, assess their size, location, and spread, enabling doctors to make informed decisions about the most effective treatment plans.
However, repeated or high-dose radiation exposure can lead to side effects such as tissue damage, increased risk of developing secondary cancers, and other long-term health issues. Therefore, healthcare professionals carefully weigh the benefits of cancer staging imaging against the risks associated with radiation exposure, ensuring that patients receive the minimum necessary dose for accurate diagnosis while minimizing potential harm.
Minimizing Risk During Diagnostic Scans
Minimizing risk during diagnostic scans is a crucial consideration in cancer care, especially for cancer staging imaging. While advanced imaging techniques like CT, MRI, and PET scans provide vital information for accurate diagnosis and treatment planning, they also expose patients to ionizing radiation. Healthcare professionals are tasked with balancing the benefits of these scans against potential risks of excessive radiation exposure.
Strategies to minimize risk include using lower-dose protocols when possible, employing alternative imaging methods where appropriate, and adhering to strict protocol guidelines. Additionally, regular monitoring of radiation doses and patient history can help ensure that each scan is justified and performed safely, contributing to the overall effectiveness of cancer treatment while safeguarding patient well-being.
Future Directions to Enhance Safety Measures
As technology advances, future research should focus on developing safer alternatives for cancer staging imaging. One promising direction is implementing advanced radiation-reducing techniques, such as optimized protocols and improved scanning equipment, to minimize exposure while maintaining diagnostic accuracy. Additionally, exploring alternative contrast agents or molecular targeting approaches could offer non-ionizing radiation options, further reducing health risks.
Integrating artificial intelligence (AI) into image analysis is another strategic move. AI algorithms can assist radiologists in detecting subtle abnormalities and enhancing visualization, potentially lowering the need for repeat scans and thus reducing overall exposure. Moreover, personalized medicine approaches tailored to individual patient needs may become more prevalent, ensuring that cancer staging imaging optimizes diagnostic benefits while minimizing potential long-term effects on patients’ health.
Cancer diagnostic scans, while essential for accurate cancer staging, require careful consideration due to radiation exposure risks. Understanding the benefits and minimizing potential harm through advanced techniques and stringent safety measures is crucial. Future research into less invasive and more precise imaging methods holds promise for enhancing patient safety without compromising diagnostic accuracy in cancer staging.